Admission
Home
Work in progress!
Hypoglycaemia Flowchart
Home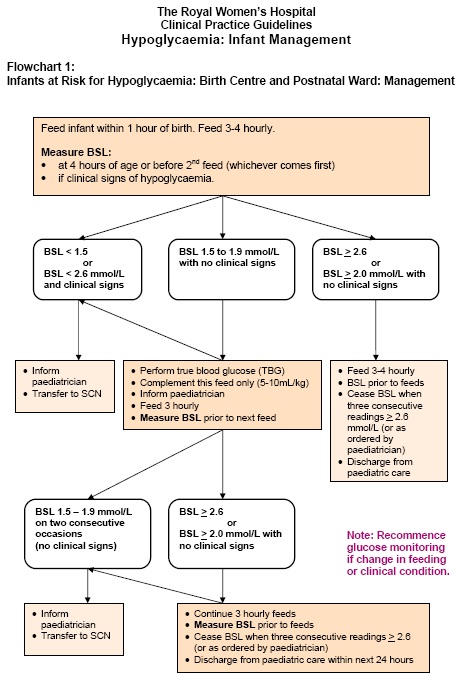
Jauindice 27 weeker
Home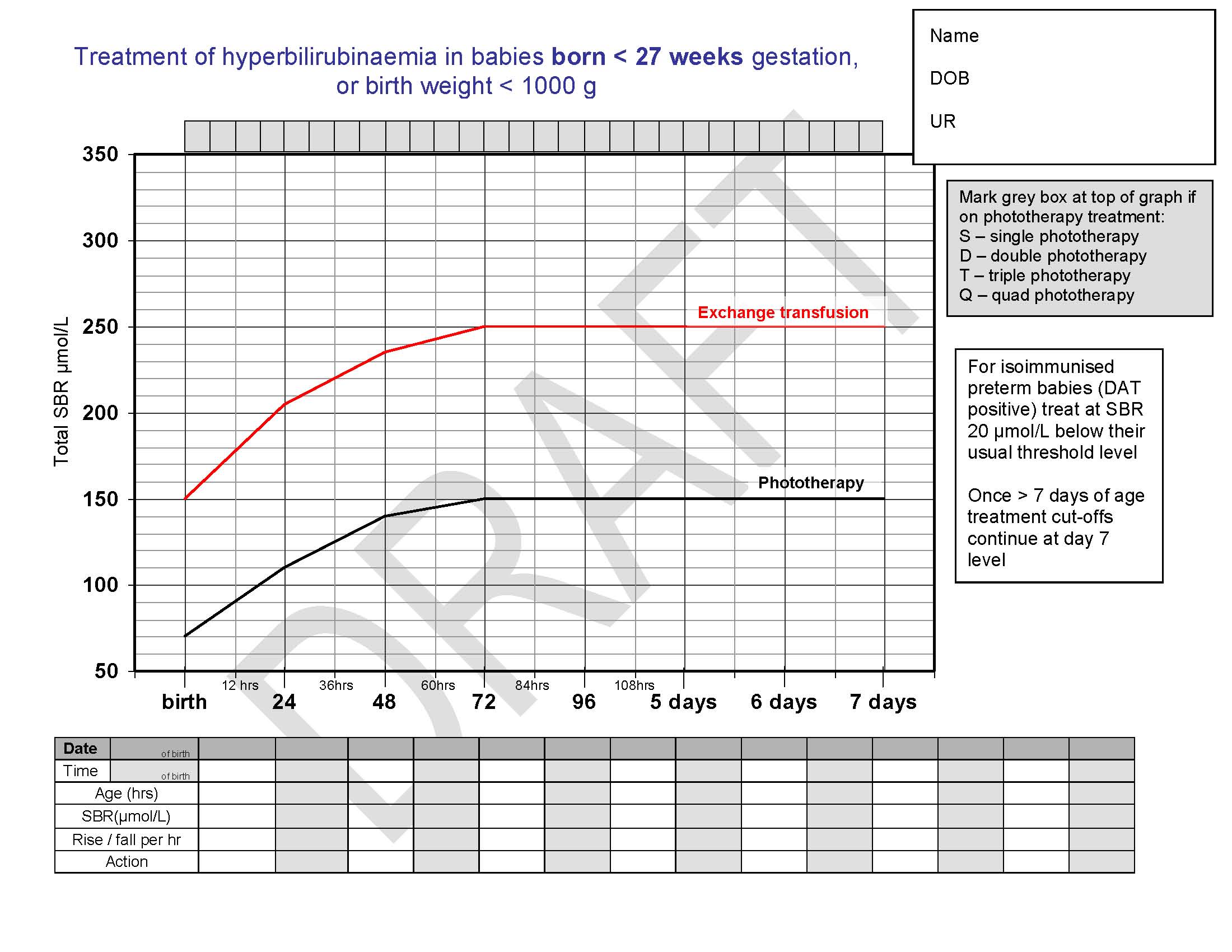
Cranial US
Home
Cranial ultrasounds are performed routinely on preterm
neonates.
After a review of the database, plus
the literature we have modified
the usual routine for minimum surveillance cranial ultrasounds.
|
Gestation |
Day 0-1 |
Day 7-10 |
Day 28 |
Day 60 |
Day 90 |
|
30-31+6 |
no |
yes |
no |
no |
no |
|
28-29+6 |
no |
yes |
yes |
yes |
no |
|
Less than 28 weeks |
yes |
yes |
yes |
yes |
yes |
Clinical indicators for a non-routine cranial USS:
- Preterm infants with chorioamnionitis demonstrated on placental pathology
- Meningitis
- Neonatal encephalopathy: HIE, seizures or metabolic
- Antenatal cranial abnormality or bleeding diathesis
- Significant deterioration where intracranial pathology is suspected: Hypotension Pneumothorax
Further imaging following the diagnosis of intracranial pathology will be dependant.by the clinical picture.
DATE: 28/09/12
Admission
HomeThere is a lack of consensus on a definition of neonatal hypoglycaemia. It is recommended that clinical practice be guided by operational thresholds (i.e. blood glucose levels at which clinical interventions should be considered).
Clinical signs which suggest clinically significant hypoglycaemia are non-specific and include jitteriness, irritability, high pitched cry, cyanotic episodes, apnoea, seizures, lethargy, hypotonia or poor feeding. Many babies with hypoglycaemia will have no clinical signs.
Operational thresholds on Post-natal wards:
- Infant with risk factors for hypoglycaemia but no clinical signs - blood sugar level < 2.0 mmol/L
- Infant with clinical signs: blood sugar level < 2.6 mmol/L.
- All infants - true blood glucose < 2.6 mmol/L.
True Blood Glucose (TBG): as measured on a blood gas analyser in Newborn Intensive and Special Care or by laboratory measurement.
2. Responsibility
All medical and nursing staff caring for newborn infants, including infant of a mother who has diabetes.3. Process
Do not measure blood glucose levels in well, term infants.Monitor infants with risk factors for hypoglycaemia, including:
a. maternal indications:
- mother who has diabetes.
- small for gestational age infants (< 10th centile), low birthweight infants (< 2,500gm) or clinically wasted regardless of birthweight
- macrosomic or large for gestational age infants (> 90th centile)
- infants admitted to Newborn Intensive and Special Care with:
- CNS depression at birth or encephalopathy
- rhesus isoimmunisation
- polycythaemia
- sepsis
- respiratory distress
- prematurity
- nil orally
Infants of mothers who have diabetes
Inform paediatric registrar of impending birth of an infant of a mother who has diabetes. After birth, paediatric registrar to decide whether the infant should be managed in the postnatal ward or Newborn Intensive and Special Care.Transfer infant of a mother who has diabetes to Newborn Intensive and Special Care if:
a. maternal indications:
- poor control during pregnancy (most recent HbA1c > 7.5%)
- BSL > 8 mmol/L during labour
- IV glucose during labour.
- unwell (e.g. signs of respiratory distress)
- macrosomic (> 90th centile)
- small for gestational age infants (< 10th centile), low birthweight infants (< 2,500gm) or clinically wasted regardless of birthweight
- preterm (< 37 weeks gestation)
- other reason(s) for addmission to Newborn Intensive and Special Care.
All other well infants of mothers who have diabetes (type 1, type 2 or gestational diabetes, controlled by insulin or diet) should be transferred to the postnatal ward with their mother. Refer to: Management of infants at risk for hypoglycaemia in Birth Centre and postnatal wards and Flowchart 1 (Appendices) in this procedure.
Note: Mother managed with insulin prior to or during pregnancy is not an indication alone for transfer of infant to Newborn Intensive and Special Care.
For management of infants transferred to Newborn Intensive and Special Care, refer to: Management of infants with risk factors for, or diagnosis of hypoglycaemia in Newborn Intensive and Special Care and Flowchart 2 (Appendices) in this procedure.
Management of infants at risk for hypoglycaemia in Birth Centre and postnatal wards
Flowchart 1: Infants at Risk for Hypoglycaemia - Birth Centre and Postnatal Ward (LINK)
Commence feeding within one hour of birth and feed 3 - 4 hourly.Measure Blood Sugar Level (BSL):
- at four hours of age or before the second feed (whichever comes first)
- if clinical signs of hypoglycaemia present
- before each subsequent feed until 3 consecutive readings ≥ 2.6 mmol/L, or as requested by paediatric registrar.
Note: Confirm any BSL reading < 2.0 mmol/ L (infant with no clinical signs) or < 2.6 mmol/L (infant with clinical signs) with a TBG (laboratory) measurement. Do not wait for result before responding.
If BSL is 1.5-1.9 mmol/L in infant with no clinical signs:
- inform paediatric registrar
- complement this feed only with EBM/formula (5-10mL/kg/feed)
- feed infant 3 hourly
- continue to measure BSL before feeds.
- any BSL < 1.5 mmol/L
- any BSL < 2.6 mmol/L and clinical signs
- 2 consecutive BSL 1.5-1.9 mmol/L (no clinical signs).
Infants may be discharged from paediatric care after 3 consecutive BSL ≥ 2.6 mmol/L.
Paediatric registrar to review infants daily until discharge from paediatric care.
Infants managed for hypoglycaemia in the postnatal ward do not require routine neonatal outpatient follow-up.
Management of infants with risk factors for, or diagnosis of hypoglycaemia in Newborn Intensive and Special Care
Flowchart 2: Infants admitted - Newborn Intensive and Special Care with risk factors / diagnosis hypoglycaemia (LINK)
Measure TBG on blood gas analyser:- within one hour of arrival in nursery (or as ordered by paediatric registrar)
- if TBG ≥ 2.6 mmol/L repeat before next feed, or 3 hourly if infant nil orally
- if TBG < 2.6 mmol/L- repeat TBG in 1 hour
- measure TBG before feeds if feed due
- glucose monitoring may be discontinued when 3 consecutive TBG readings ≥ 2.6 mmol/L
- recommence glucose monitoring if indicated when change in feeding regime or clinical condition.
TBG ≥ 2.6 mmol/L:
- feed by 1 hour of age (60mL/kg/day) with EBM if available, or formula
- feed 3 hourly (if birthweight > 1.5kg)
- complement breastfeeds with EBM/formula (30-60mL/kg/day)
- if there is any contraindication to enteral feeds - insert IV and commence 10% glucose infusion at 60mL/kg/day (4mg/kg/min).
TBG 1.5 - 2.5 mmol/L:
- feed 2 hourly (60mL/kg/day)
- commence feeding within 1 hour of admission with EBM if available, or formula
- if repeat TBG is 1.5-2.5 mmol/L increase feeds to 90ml/kg/day
- change to 3 hourly feeds (if birthweight > 1.5kg) after 24 hours of age if at least 2 consecutive blood glucose readings ≥ 2.6mmol/L
- complement breastfeeds with EBM/formula (60-90mL/kg/day)
- if there is any contraindication to enteral feeds - insert IV and commence 10% glucose infusion:
- AGA infant - 70mL/kg/day (5mg/kg/min), increasing to 90mL/kg/day (6mg/kg/min) if subsequent TBG < 2.6 mmol/L
- SGA infant - 90mL/kg/day (6mg/kg/min), increasing to 120mL/kg/day (8mg/kg/min) if subsequent TBG < 2.6 mmol/L.
TBG <1.5 mmol/L:
consider an intramuscular injection of glucagon for infants ≥ 34 weeks gestation with adequate glycogen stores (birthweight > 10th centile) - refer to Pharmacy Manual. This will increase blood glucose whilst IV is inserted and 10% glucose infusion commenced.- insert IV and commence 10% glucose infusion:
- AGA infant - 70mL/kg/day (5mg/kg/min), increasing to 90mL/kg/day (6mg/kg/min) if subsequent TBG < 2.6 mmol/L
- SGA infant - 90mL/kg/day (6mg/kg/min), increasing to 120mL/kg/day (8mg/kg/min) if subsequent TBG < 2.6 mmol/L.
- administer IV bolus of 2ml/kg 10% glucose (200mg/kg) over 3-5 minutes.
TBG 1.5-2.5 mmol/L despite feeding regime:
consider an intramuscular injection of glucagon for infants ≥ 34 weeks gestation with adequate glycogen stores (birthweight > 10th centile) - refer to Pharmacy Manual. The decision to insert an IV may be delayed until result of next TBG (repeated in 1 hour or as ordered by paediatric registrar).OR
insert IV and commence 10% glucose infusion at 90mL/kg/day (6mg/kg/min). (Do not administer IV bolus of 10% glucose if TBG ≥ 1.5mmol/L.
Calculate and document IV glucose infusions in mg/kg/min.
Continue enteral feeds as tolerated and support breastfeeding (do not make nil orally unless enteral feeding contraindicated).
Increase feeds gradually and gradually reduce IV glucose infusion when TBG readings are stable (at least 2 consecutive readings ≥ 2.6mmol/L).
Infants on 3 hourly sucking feeds may be discharged to postnatal ward as soon as BSL ≥ 2.6 mmol/L on 3 consecutive occasions. If hypoglycaemia has occurred, complementary feeds after breastfeeding may be necessary for a day or two until maternal milk supply is established. Infant admitted to SCN for management of hypoglycaemia to remain under paediatric care in postnatal ward for at least 72 hours.
Only infants admitted to NISC for management of hypoglycaemia who receive IV glucose for more than 3 days, and/or glucagon infusion, and/or diazoxide will be reviewed in the general neonatal outpatient clinic.
Persistent hypoglycaemia
Glucagon injection may be repeated once if initial response was good (TBG ≥ 2.6 mmol/L).Increase rate of IV 10% glucose infusion (up to 150mL/kg/day - 10mg/kg/min).
- IV fluids must not be increased > 120mL/kg/day in the first 24 hours
- if fluid restriction necessary, increase glucose concentration.
If persistent hypoglycaemia in spite of increased glucose infusion rate/concentration, discuss with Paediatric Consultant and consider:
- intravenous infusion of glucagon
- administration of hydrocortisone.
Suspected hyperinsulinism
Diagnosis:- macrosomia
- glucose infusion rate >10mg/kg/min
- hypoglycaemia persists after day 3.
When TBG < 2.0mmol/L collect arterial or venous blood for:
- glucose
- insulin
- growth hormone
- cortisol
- free fatty acids
- urine for ketones and organic acids.
- ammonia
- acyl-carnitine
- lactate.
- Aim for TBG > 3.0 mmol/L.
- Consider ceasing enteral feeds (as may stimulate insulin release).
- Discuss specific management with Endocrinologist.
Appendices
Appendix 1: Flowchart 1: Infants at Risk for Hypoglycaemia - Birth Centre and Postnatal WardAppendix 2: Flowchart 2: Infants admitted to Newborn Intensive and Special Care with risk factors / diagnosis hypoglycaemia
5. Reference documents
Victorian Neonatal Handbook, 2005 http://www.netsvic.org.au/nets/handbook/index.cfmHypoglycaemia http://www.netsvic.org.au/nets/handbook/index.cfm?doc_id=631
Infant of the Diabetic Mother (IDM) http://www.netsvic.org.au/nets/handbook/index.cfm?doc_id=889
Cornblath M. et al, Controversies regarding definition of neonatal hypoglycemia: Suggested Operational Thresholds. Pediatrics 2000; 105:1141-45
Deshpande S, Ward Platt M. The investigation and management of neonatal hypoglycaemia. Seminars in Fetal & Neonatal Medicine 2005;10:351-361
Roberton's Textbook of Neonatology, Rennie JM (Ed), 2005, 4th edition
The Royal Women's Hospital Clinician's Handbook, 2006, Intensive and Special Care Nurseries.
Williams A F. Neonatal hypoglycaemia: Clinical and legal aspects. Seminars in Fetal & Neonatal Medicine 2005;10:363-368
Revised & updated: 20 April 2009.